WHAT IS IT?
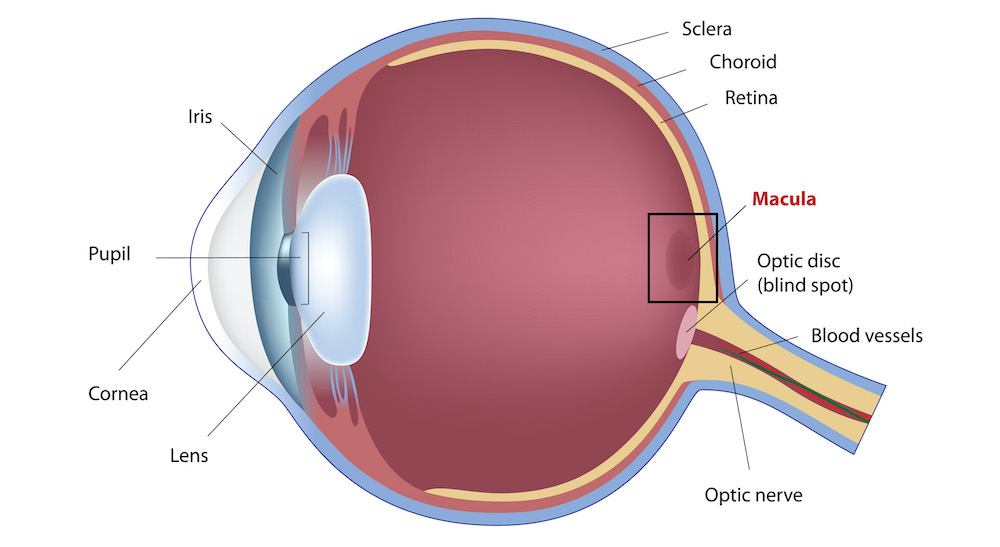
A macular hole is the name for the formation of a break in the centre of the retina, the area which call the macula. It usually occurs in people over the age of 50 and it is more common among women. It can be bilateral in 15% of individuals.
Its diagnosis is clinical, i.e., viewing the back of the eye after dilating the pupils and using magnifying lenses. However, in all cases, we will perform a scan of the macula (OCT or optical coherence tomography) to measure the size and thickness of the macular hole, upon which will depend the prognosis and potential treatment.
SYMPTOMS
The clinical signs of a macular hole can vary: from patients who are completely asymptomatic at the start to a severe loss of vision and the appearance of a blind spot in the centre of the eye (scotoma).
Metamorphopsia (perception of distorted images and straight lines with undulations) is also very common as is macropsia and/or micropsia (seeing objects as larger or smaller than they are in reality).
A very characteristic symptom of this condition is seeing broken lines, known as the “Watzke-Allen sign”.
CAUSES AND RISK FACTORS
It is believed that its cause lies in the traction that the vitreous humour (transparent gelatinous liquid filling the eyeball) exercises over the macula when it contracts, because of a physiological ageing process. Under normal conditions, when we get older, the vitreous detaches, i.e., the intraocular gel recedes and moves away from the macula without causing any damage thereto or having any consequences on the eyesight. However, in some people, the vitreous cortex has strong adherence to the macula and a sharp focal contraction thereof leads to a break in the macular tissue and the formation of a macular hole.
We can also experience a macular hole after a blunt eye trauma, in the context of a high degree of myopia or a chronic macular oedema complication.
TYPES
Macular holes can be classified in different ways:
— According to their cause: Idiopathic or senile (associated with ageing), myopic (those that occur to patients with a high degree of myopia) and traumatic (the consequence of previous trauma).
— According to the thickness of the damaged retina: Full-thickness (when the hole affects the full thickness of the retina) and lamellar (when they partially affect the thickness of the retina) associated, in general, with the epiretinal membrane.
— According to the OCT findings: A complex classification that we do not mention herein.
PREVENTION
There is no way of preventing a macular hole from forming. What is important, however, is diagnosing it at a very early stage when surgery is very effective. Therefore, regular eye check-ups, above all in patients who have had the same condition in the contralateral eye, are advised.
TREATMENT
Macular hole treatment is eminently surgical.
The surgery is called a vitrectomy . It is an outpatients procedure and performed under local anaesthesia. It’s a microincision technique, i.e., it uses microscopic incisions that do not require stitches. It involves removing all the structures that cause traction on the macula, be it the vitreous humour, the epiretinal membrane or the internal limiting membrane of the retina (the outermost layer of the retina).
At the end of surgery, a gas bubble is injected into the vitreous cavity (intraocular tamponade), which helps the macular hole to close. For the days following surgery, patients will have to stay in quite a strict position (generally seated or with the mouth facing downwards), depending on the type of duration of the gas.
The surgical outcomes are more promising the less the disease has evolved and the smaller the size of the hole. In early cases, there is a high percentage of anatomical closure and a considerable improvement in visual acuity compared to more advanced cases or macular holes in myopic eyes.
PROFESSIONALS WHO TREAT THIS PATHOLOGY
- Dr. Santiago Abengoechea
- Dr. Mª José Capella Elizalde
- Dr. Javier Elizalde
- Dr. Jeroni Nadal
- Dr. Sònia Viver