WHAT IS LATERAL APPROACH XLIF
Extreme Lateral Interbody Fusion (XLIF) is a recently available, innovative technique for lumbar fusion surgery, that makes it possible access the spinal column using a lateral path through the outermost part of the abdomen. Once the spine has been reached, with this technique, it is possible to manipulate the discs and vertebrae while avoiding damage to the nerves and muscles.
Since its introduction, this technique has been widely used in the United States, and gradually extended through Europe, where we pioneered its use when Dr. Francesco Caiazzo was the first surgeon to use it in Spain, in 2014, with the XLIF Nuvasive system.
The procedure consists of a transpsoas retroperitoneal approach that gives direct access to the intervertebral disc from an antero-lateral view, allowing almost complete replacement of the disc and correction of the sagittal plane. It allows the entire lumbar spine to be accessed up to the 5th lumbar vertebra (L5, except the lumbosacral transition L5-S1), and the thoracic spine up to the 4th thoracic vertebra (T4).
WHICH CASES IS IT USED FOR?
This technique is used to perform intervertebral arthrodesis or fusion [enlace a fusión] and is used especially when dealing with degenerative pathologies of the spinal column, such as:
- Degenerative disc disease (DDD).
- Spinal stenosis and foraminal stenosis.
- Spondylolisthesis (vertebral displacements), both from degenerative disease and from other causes (injury, congenital, acquired, etc.).
- Surgical repair of failed prior surgeries.
- Pathology in the adjacent segment.
- Deformities: adult degenerative scoliosis, FBSS-failed back surgery syndrome and alterations of sagittal balance.
When the segments affected by the pathology are between the 4th thoracic vertebra (T4) and the 5th lumbar vertebra (L5), except the L5-S1 space, this approach is also used to perform arthrodesis of thoracic segments, up to T4, and to treat thoracic disc herniations and thoracic-lumbar vertebral fractures.
WHAT DOES THE PROCEDURE CONSIST OF?
The technique consists of two parts: first, the approach, and second, the arthrodesis itself.
Approach
With the patient lying on one side, the surgeon makes a lateral incision, usually horizontally, to access the muscles of the abdominal wall. Next, the muscle fibers are separated (without cutting them) from the external oblique, internal oblique and transverse muscles of the abdomen. Once past the transverse muscle of the abdomen, the retroperitoneal space is accessed, where the psoas muscle is identified. Using specific instruments, we pass through this muscle, performing neurophysiological mapping to identify the nerves in the muscle so as not to harm them. A separator is then placed that allows us to access the intervertebral disc.
Arthrodesis
The diseased intervertebral disc is cut out. Usually, this access is used for the upper lumbar segments up to L4-L5, except for the L5-S1 space. Once the disc is completely removed, the vertebral endplates are cleaned, removing the cartilage, so that the arthrodesis material can more easily contact and fuse with the bone of the vertebra. Once the disc space has been prepared, the interbody fusion cage, or “spine cage” can be placed (it can be made of a variety of materials such as titanium, porous titanium or PEEK- Polyetheretherketone, titanium-coated PEEK, NanoMetalene etc..).
These materials have the characteristics of driving the fusion, that is to say, they guide the formation of the bone callus between the two vertebrae. Usually, to facilitate the formation of this callus, the “cages” are filled with a material referred to as bone wax, which may be of various origins. These are biological materials, which, in addition to helping and guiding the formation of the callus, they generate and stimulate formation of bone. After the fusion takes place, the surgery is usually completed with the placement of posterior screws that will be implanted in a minimally invasive percutaneous way, to give greater stability to the fused vertebrae.
ADVANTAGES OF EXTREME LATERAL INTERBODY FUSION (XLIF)
Minimally aggressive approach
Minimally aggressive towards functional structures thanks to the minimally invasive percutaneous approach.
Recovery
Less pain and faster recovery: the surgical access is made using a retroperitoneal approach, cutting no muscles and with no aggression to the patient’s bone.
Reduced hospital stay
Reduced hospital stay: in the absence of any complications the blood loss is minimal compared to a classic posterior approach.
Better results
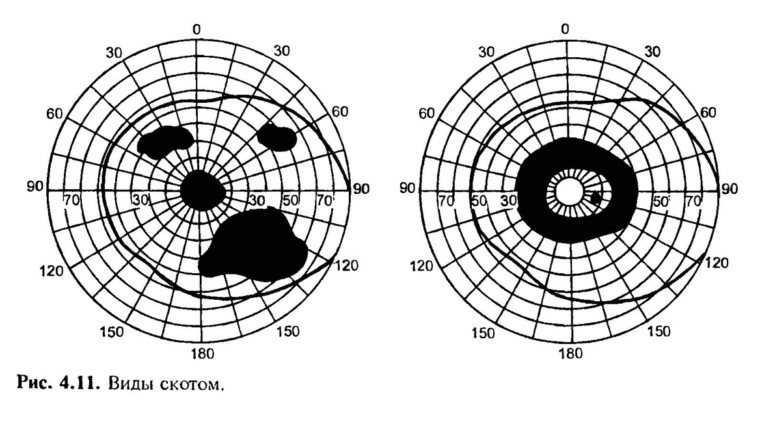
The interbody cages used in this procedure, are larger and wider than any others, so they allow bicortical support and they occupy a larger area of contact between the vertebrae. This, in turn, means that they offer a much more powerful biomechanical support than any other prosthesis, and above all, better fusion and stability results compared to PLIF (posterior lumbar interbody fusion) and TLIF (transforaminal lumbar interbody fusion), which are techniques for disc stabilization using a posterior approach. This improves the stability of the patient’s spine.

TLIF PLIF XLIF
(photo source: Nuvasive)
THE PATIENT CAN RETURN TO WORK AND NORMAL DAILY ACTIVITIES SOONER
The cage used in a lateral approach gives a much wider area of surface contact between the vertebrae than a cage placed by any other surgical approaches. It has been shown that in order to create a good fusion environment between two vertebrae, and allow them to fuse to each other, the interbody cages should cover at least 30% of the surface of the vertebrae (the so-called vertebral endplate); prostheses inserted by the XLIF route sometimes cover more than 50% of the usable fusion surface between 2 vertebrae. If complemented with posterior screws, the interbody fusion has a higher percentage of fusion compared to all other techniques, both anterior and posterior.
MAINTAIN THE PATIENT’S SAGITTAL BALANCE
The XLIF system, offers cages of different angles and lordosis (0, 10, 20, 30 degrees). It is scientifically proven that the placement of hyperlordotic interbody cages using the ACR (Anterior Column Realignment) technique is effective in surgery to correct deformities and allows the patient’s sagittal balance to be conserved, unlike complex vertebral osteotomy surgeries that require long surgical times, entail considerable blood loss, have high rates of complications and high hospital readmission rates.
RATE OF COMPLICATIONS
The rate of complications is very low: the technique is used by specialized surgeons and can be used to treat multiple pathologies.
INDIRECT DECOMPRESSION
Makes it possible to perform indirect decompression of the central spinal cord, and of the vertebral foramina in many cases. In this way we avoid performing a direct decompression which is performed following aggression and decompression of the posterior musculature, and resection of the patient’s posterior bone elements.
RECOVERY AND REHABILITATION
Following surgery, the patient is transferred to a hospital room, and the next day will already be able to begin moving about, and even walk. A follow-up EOS x-ray is taken, and on the fourth day after surgery, the patient is usually discharged.
Next, about 7 to 10 days after the operation, the patient will see a member of the nursing staff at Instituto Clavel to check how the surgical wound closure is healing. The patient may need to wear an elastic support during the first weeks after surgery.
Approximately 4 to 6 weeks after the surgery, the patient will return to the clinic for a visit with the surgeon. The patient should also have periodic follow-up x-rays taken at 3, 6, 9, and 12 months from the date of the surgery, to track how the fusion is progressing.
Depending on how the recovery is progressing, in about 3 to 6 months from the date of the surgery, the patient can gradually return to normal activities, including some specific physical activity (elliptical or stationary bike, swimming, walking on a treadmill, cardio exercise, stretching, Pilates and yoga) under the supervision and guidance of physiotherapists, like those of FisioSpine.
RISKS OF THE SURGERY
The risks and possible complications can be related to either the approach, or the arthrodesis. With respect to the approach, there may be the typical risks associated with any surgery:
- Hemorrhage
- Hematoma
- Superficial and/or deep infection
More specifically, in this surgery there is the risk of lesion to the muscle of the abdominal wall, which can cause a lump to appear in the abdominal wall. Passing through the psoas muscle may weaken the muscle, which causes discomfort in the form of pain or tingling when the hip is flexed. Usually, this discomfort is temporary (< 4 weeks) disappearing spontaneously or with the help of medication.
Rarely, in less than 1% of cases, the lumbar nerve plexus may be damaged, provoking damage in the nerve that weakens leg strength. Extremely rare, (<1%) are lesions to organs or abdominal blood vessels (veins or arteries).
With respect to the arthrodesis, we may find the following risks:
- Failure of the vertebrae to fuse (pseudoarthrosis, or non-union) which leads to recurrence of the same pain as before the surgery <5%.
- The fusion cage moves or sinks into the vertebral body < 5%
- Fracture of the vertebral endplates <1%.
If any of these circumstances arise, a new surgery may be necessary. Due to the distraction between the treated vertebrae, that is, the recovery of the disc height after implant placement, radiculopathy may appear in the postoperative period (<5%), which is usually transient and may require short-term medical treatment.